Obsessive-Compulsive Disorder is a mental health condition. In this disorder, the person has recurrent, unwanted thoughts (obsessions) and behaviours (compulsions). These compulsions and obsessions take up a lot of time, disrupt daily life, and cause a great deal of distress. A vicious cycle of anxiety seems to keep these people entangled, wherein their thoughts create that anxiety. Besides, it would also repeat some actions to reduce anxiety.
OCD is not a normal habit. The thoughts are not just ordinary worries, and the actions are not something that an individual can easily control. This issue can affect children, teens, and adults and may significantly affect all aspects of a person's life.
Obsessions refer to unwanted, intrusive thoughts, images, or urges that evoke discomfort or anxiety. They may be irrational or distressing to the person experiencing them. Common signs of obsession include:


Repeated actions or thoughts carried out in reaction to an obsession are known as compulsions. Usually, these behaviours are carried out to lessen anxiety or stop a feared situation. A few common compulsion indications are:
Checking: Checking locks, appliances, or light switches just to ensure they are okay.
Cleaning: Repeated hand-washing, cleaning of items, and even cleaning the environment to an extreme degree.
Counting or Repeating Behaviors: Acting the same way several times or repeating himself to make sure it is just right.
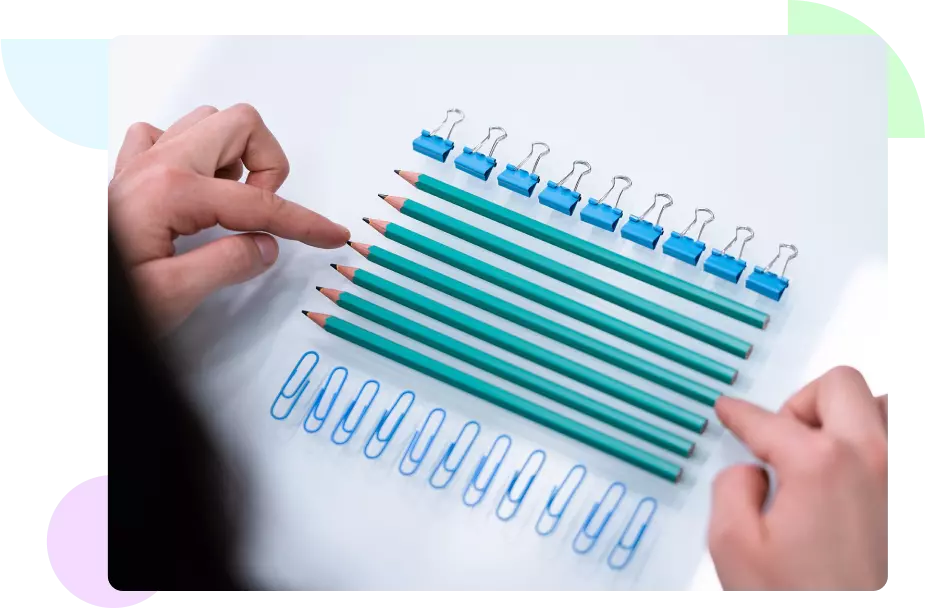
Arranging and Organizing: Aligning objects or preparing items in a very specific order or pattern to alleviate discomfort.
OCD can have many different looks depending on the type of obsessions and compulsions. The following are common types of OCD:
Symmetry and Ordering OCD: Impulsive need for symmetry or order about objects, actions, or thoughts.
Checking OCD: Repeated checking of things like locks, appliances, or even one's self from harm or disaster.
Intrusive Thoughts OCD: Intrusive, unwelcome thoughts that are generally violent, sexual, or morally inappropriate.
Contamination OCD: It is a fear of germs, dirt, or chemicals that causes a person to keep cleaning or avoid places to prevent contamination.
Hoarding OCD: The inability to get rid of certain things because one fears losing an important item or feeling intense anxiety when considering the act of getting rid of things.

A mental health professional will scrutinize the patient's symptoms, medical history, and behaviour. In a nutshell, the process of diagnosing can be the following way:
Clinical Evaluation: The doctor will ask the client several questions regarding their thoughts, feelings, and behavioural changes. In this stage, he tries to understand the pattern of obsessions and compulsions.
Psychological Assessment: At times, a psychological test may be conducted to determine the severity of OCD signs. This would inform the level of interference of the disorder in one's daily life.
Physical Examination:OCD falls under mental illness. However, a physical examination may be administered to eliminate other underlying medical conditions that may cause such indications to develop.
General treatment of OCD is a combination of therapy, medication, and lifestyle changes. However, here are some of the most effective treatments:
Cognitive Behavioral Therapy (CBT): Cognitive Behavioral Therapy (CBT) effectively treats OCD by addressing distorted thinking. A key technique, Exposure and Response Prevention helps clients face anxiety without performing compulsions, reducing both over time.
Medications: Selective serotonin reuptake inhibitors (SSRIs), including fluoxetine (Prozac), sertraline (Zoloft), and fluvoxamine (Luvox), are commonly prescribed to manage OCD by enhancing serotonin levels, impacting mood and anxiety.
Support Groups and Therapy: Join a support group or seek therapy from an OCD specialist for emotional support and learn effective coping strategies in a safe, supportive environment.
Deep Brain Stimulation (DBS): Deep brain stimulation may help severe OCD cases by implanting a device that sends impulses to brain areas controlling mood and behavior, when medication and therapy fail.
Lifestyle Changes: Combining treatments with lifestyle changes, such as exercise, mindfulness, balanced sleep, and nutrition, can help manage OCD and reduce stress, caffeine, and alcohol intake.

